Why Do Some People Get Sick All the Time, While Others Stay in Freakishly Good Health?
This at first appeared in the July/August difficulty of Discover journal as “Titans of Immunity.” Assist our science journalism by starting to be a subscriber.
For a long time, Melanie Musson’s mates have marveled at her superpower: staying healthier no issue what germs are creating the rounds. Colds and flu felled a great deal of Musson’s dormmates in college or university, but the viruses often appeared to pass her by. “I in no way acquired ill at the time,” she claims. “I acquired about five hrs of slumber a night time, I concluded school in a few a long time, and I labored thirty hrs a week in the course of. My finest mates labeled me ‘the equipment.’ ”
Musson’s ironclad immune program also established her aside at her very first work. While she was doing work at an assisted dwelling facility, her co-employees succumbed to a belly virus that was functioning rampant. Undaunted, Musson provided to go over their shifts. “There I was, the model-new staff, acquiring as considerably time beyond regulation as I wished. I was not worried that I’d catch [the virus], due to the fact it just does not come about.”
While the rest of us battle seasonal flu, chronic allergy symptoms and back-to-back wintertime colds, Musson and other immune masters glide via with scarcely a sniffle — one thing University of Pittsburgh immunologist John Mellors sees all the time. “People get exposed to the same virus, the same dose, even the same resource. 1 gets pretty ill, and the other does not.”
It is only organic to wonder: Why do some people often feel to tumble on the proper aspect of this equation? And could our have immune devices technique the same degree with the proper tuneup?
Medical doctors have observed organic variants in the immune reaction among the people since Hippocrates’ time, but the motives remained elusive for hundreds of years. New research, however, is starting up to illustrate just how your genes, behaviors and earlier disease exposures have an impact on the character and toughness of your immune reaction. These discoveries are serving to to determine the parameters of a race in which people like Musson have a head start off — and other individuals have considerably more floor to go over.
In the Genes
The minute a virus, bacterium or other invader breaches your cells’ walls, your overall body rolls out a tightly choreographed protection method. The most important architects of this system are a established of human leukocyte antigen (HLA) genes, which code for molecules that fine-tune the body’s immune reaction. So when a bacterium gets into just one of your cells, your HLA genes churn out proteins that flag the mobile as infected so that specialised immune cells will swarm in to wipe out it. Other HLA genes activate cells that rein in the immune reaction, so it does not wipe out more than essential.
Like fingerprints, everyone’s HLA gene assortment is distinctive. Your HLA genes give you a wide repertoire of immune protection ways, but “that repertoire may well be excellent for some microorganisms and lousy for other individuals,” Mellors claims. “It’s not like there’s just one HLA kind that’s hugely immune to anything.” This genetic variation can help clarify why you could catch every cold virus going about but haven’t gotten a belly bug in decades. A Massachusetts Standard Clinic analyze found that some so-named HIV controllers — immune stalwarts who never create AIDS from the virus HIV — have HLA gene variants that prompt specialised cells to swarm in and attack proteins important to the virus’ functionality.

(Credit: Shutterstock)
But your HLA genes are not the only ones that condition your immune resistance. The Human Genome Task has discovered tens of hundreds of gene variants that are more popular in people who create precise disorders and much less popular in people with out these problems.
Flagging these forms of gene-disease back links is a comparatively basic issue, claims immunologist Pandurangan Vijayanand of the La Jolla Institute for Immunology. After researchers discover a gene sequence that’s joined to disease, however, they require to “figure out what it is basically doing,” claims Vijayanand. “How is this alter in the sequence impacting the mobile or producing the susceptibility [to disease]?”
To answer this issue, Vijayanand and his team are producing what they contact an atlas, to catalog which proteins each individual gene provides and how these proteins alter the functionality of various mobile types. For case in point, he has discovered a gene variant that makes people more susceptible to asthma — a affliction in which the overall body attacks its have healthier airway cells — by driving higher creation of proteins that rev up the immune reaction. Other gene variants seem to assistance people fight lung tumors by prompting their tissues to produce more T lymphocytes, specialised immune shock troops that eliminate most cancers cells.
While a dizzying selection of genetic discrepancies stay to be cataloged, immunologists agree that, in basic, these discrepancies assistance clarify why resistance to some pathogens can feel to operate in people. People today like Melanie Musson probably get a genetic leg up to some diploma — Musson claims her mom, father and siblings hardly ever get ill. Conversely (and unfairly), you could as an alternative inherit a inclination to create diabetic issues, recurrent strep infections or autoimmune disorders.
Context Matters
On the other hand anemic or hardy your innate immune arsenal, it provides only the wide contours of your body’s resistance to threats. Environmental influences fill in the specifics, from wherever you reside to your sleeping patterns to your heritage of prior infections.
In a 2015 Cell analyze, researchers researched more than 100 pairs of equivalent twins and how their immune devices responded to the flu shot. About a few-quarters of the discrepancies they saw were being pushed by environmental factors rather than genetic ones. The discrepancies in twins’ immune devices also grew more pronounced the older they acquired, suggesting that outside the house influences keep on to condition our immune prospective about time.
Some of these influences clearly show up in early childhood and may well be tough to offset later on. Scientists have long identified that young children who reside on farms are much less probable to create autoimmune disorders like asthma and allergy symptoms. An Ohio State University analyze from July 2019 hints at just one purpose why: Farm little ones have a more numerous array of gut microbes than city little ones, and the existence of some of these gut microbes predicts reduced frequencies of immune cells that create allergic irritation. Wide microbial publicity, in limited, appears to train the immune program not to overreact to substances like animal dander.
But regardless of wherever you grew up, if you are unfortunate sufficient to catch specific disease-producing bugs, they can toss your immunity off balance for a long time. Cytomegalovirus, a relative of the virus that triggers chicken pox, phases its attack by reprogramming the human immune program. Some of the virus’ proteins latch on to specific immune cells, interfering with their means to fight invaders. Other proteins, according to research from the University Clinical Middle Utrecht, interfere with the expression of important human HLA genes. And since cytomegalovirus infections are chronic, the ensuing immune deficits can go on indefinitely.
An Elective Arsenal
Obviously, you just cannot manage wherever you are raised or what random pathogens you purchase. But you can manage your day by day schedule, what you set into your overall body and how you protect your self from germs. In recent a long time, scientists have started a whole-fledged drive to come across out which lifestyle behaviors basically foster a strong immune program — and which may well be more buzz than substance.
While the over-all image of how food plan styles immunity is nonetheless blurred, new studies do hint at the immune-strengthening consequences of specific types of foods. Garlic, for occasion, incorporates a sulfur compound named allicin, which spurs creation of disease-battling immune cells like macrophages and lymphocytes in reaction to threats.
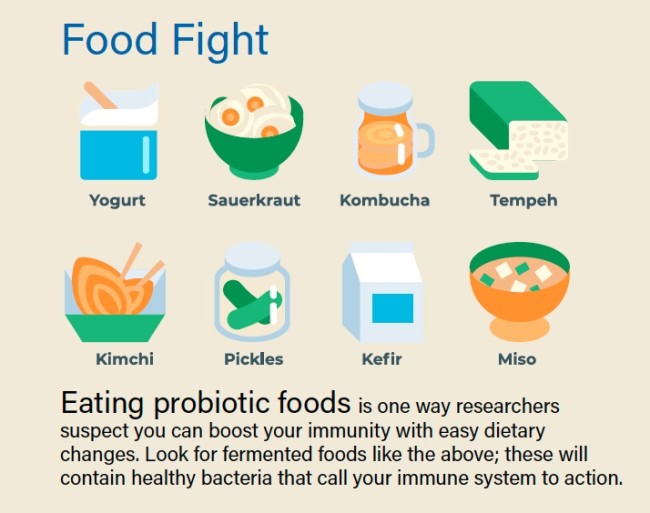
(Credit: Blessed_Find/Shutterstock)
Scientists also report that precise microbes-made up of foods — these as sauerkraut, kimchi and kefir — produce an immunologically active substance named D-phenyllactic acid. This acid appears to signal immune cells, named monocytes, to report for obligation by binding to a receptor protein on the cells’ surfaces. When people try to eat sauerkraut, “very before long afterward, we see in the blood that there’s an boost in the degree of this substance,” claims Leipzig University biologist Claudia Stäubert. In long run studies, she hopes to make clear specifically how the acid has an effect on monocytes’ exercise in the overall body.
In addition to tweaking their meal plans, numerous titans of immunity embark on intense work out regimens to hold their wellbeing strong. “I swim and snorkel 12 months-round in the ocean, up to a mile at a clip, from New England to Miami and a couple secluded points in among,” claims Baron Christopher Hanson, a business consultant who claims he just about in no way gets ill. But so significantly, scientific proof that work out enhances immunity is restricted. While a new analyze in rats demonstrates that common work out changes the prevalence of various types of immune cells, it isn’t very clear whether these changes make you much less probable to get ill.
Acquiring your day by day quota of shut-eye, however, does feel to improve your immunity. Recurring studies clearly show that slumber revs up your immune reaction, and a recent just one from Germany’s University of Tübingen stories that it does so in part by preparing disease-battling T cells to do their careers more correctly. That is due to the fact your overall body churns out more integrins — proteins that assistance T cells connect to germ-infected cells and wipe out them — although you are asleep.
But although acquiring more slumber could assistance snap your streak of wintertime colds, squirting your palms with hand sanitizer may well not. In quite a few studies, basic old soap and water was shown to eliminate germs far better than sanitizer does. “Hand sanitizer is excellent for alcoholic beverages-inclined bugs, but not all bugs are inclined,” Mellors points out. What’s more, employing sanitizer will not have any long lasting consequences on your immunity. The minute you touch a different germy floor, your slender layer of security will vanish.

Acquiring a great deal of slumber is just one way to improve your immune wellbeing: The overall body preps disease-battling cells although you are asleep. (Credit: Realstock/Shutterstock)
Placing a Stability
Champions of immunity are likely to credit score their day by day behaviors with maintaining them healthier. But numerous have also lucked into an great balance among effector T cells, the frontline immune troopers that fend off pathogens, and regulatory T cells, which hold the body’s immune arsenal in check out so it will not about-answer to threats. An overactive immune program can be just as troublesome as an underactive just one — autoimmune problems like rheumatoid arthritis, multiple sclerosis and allergy symptoms all stem from an immune reaction that’s much too forceful and sustained.
Last 12 months, scientists at Kyoto University in Japan and in other places described just one prospective way to redress this kind of imbalance: turning effector T cells into regulatory T cells in the lab. Autoimmune episodes “are brought on by antigens binding to [a] receptor on effector T cells,” claims molecular biologist Shuh Narumiya, just one of the paper’s authors. When Narumiya and his colleagues employed an inhibitor chemical to block an enzyme that controls mobile progress, cells that would usually create into effector T cells turned into regulatory T cells as an alternative — a tweak that dialed down dangerous autoimmune responses in mice.
While not everyone needs these immune fine-tuning, some people could potentially advantage from a treatment based mostly on this approach, Narumiya claims. Filling out the ranks of regulatory T cells could sometime assistance hold a assortment of disabling autoimmune problems beneath manage.
Irrespective of your T mobile balance or your immune monitor report, there’s a significant dose of serendipity associated each individual time your immune program faces a threat. You could think about your self without end susceptible to the flu or sniffles, but an X-variable — a cross-country go, a dietary tweak, a new remedy — can unexpectedly realign factors and improve your immune prospective.
By the same token, no issue how stalwart your HLA gene arsenal, how sound your slumber or how scrupulous your hygiene, you can stop up knocked flat with a horrible bug when you the very least assume it. Immune wellbeing “is like a gigantic roulette wheel. You toss the ball down and wherever it lands is a issue of chance,” Mellors claims. “You have an come across with a pathogen, and at the time you get exposed, your front line is not up to snuff.” Even titans of immunity can have Achilles’ heels — and even immune devices that feel licked at the beginning can pull off not likely victories.
Who Will get Sickest From COVID-19?
It is a recurring theme of the COVID-19 crisis: Individuals infected with the virus create vastly various indicators. Some barely truly feel just about anything — a scratchy throat, if that — although other individuals spend weeks in the ICU with ravaged lungs, unable to breathe on their have. This extensive variation in how people answer to SARS-CoV-two stems, in part, from each individual person’s distinctive genetic and lifestyle factors that have an impact on their immune functionality.
(Credit: Andrii Vodolazhskyi/Shutterstock)
Genes
Researchers in Sydney and Hong Kong have found a particular gene variant tied to higher costs of extreme indicators of SARS, a coronavirus similar to the just one that triggers COVID-19. Since the novel coronavirus only recently appeared in humans, we never know specifically which genetic quirks could make us more inclined to it. Researchers are now investigating whether other precise genes could give some people better or reduced degrees of security from the virus.
Age and Immune Well being
In some older people, or in these who have underlying immune deficits from chronic problems, regulatory T cells — which ordinarily hold immune responses beneath manage — do not functionality usually. When these people get COVID-19, so-named cytokine storms may well cause excessive irritation in the lungs, leading to existence-threatening indicators. A analyze executed by researchers in China found that COVID-19 individuals with extreme health issues had reduced levels of regulatory T cells in their bloodstream. Children may well be much less susceptible to disabling indicators due to the fact their immune devices are far better controlled and they have fewer underlying problems.
Smoking Patterns
SARS-CoV-two works by using a mobile floor receptor named ACE2 to enter the cells that line your respiratory tract. New research demonstrates that in smokers, these receptors are more preva––lent in the lungs, producing more prospective entry routes for the virus. “If you smoke,” claims Boston Children’s Clinic immunologist Hani Harb, “the virus will be able to enter more cells in better quantities.”
Elizabeth Svoboda is a science writer in San Jose, California. Her most recent e book is The Existence Heroic: How To Unleash Your Most Remarkable Self.